Patient Discharge Forms
A patient discharge form, sometimes referred to as a patient discharge summary, is a document issued by a hospital to an admitted patient at the time of his discharge from the hospital.
Who can issue a patient discharge form?
An on-duty doctor or consultant can only decide whether the patient is ready to go home. No one other than the doctor can issue the form.
Who fills out the discharge form?
A doctor who decides the discharge of the patient and who treats the patient during a hospital stay is only authorized to fill out the form and proceed with it to the billing department through the nursing staff.
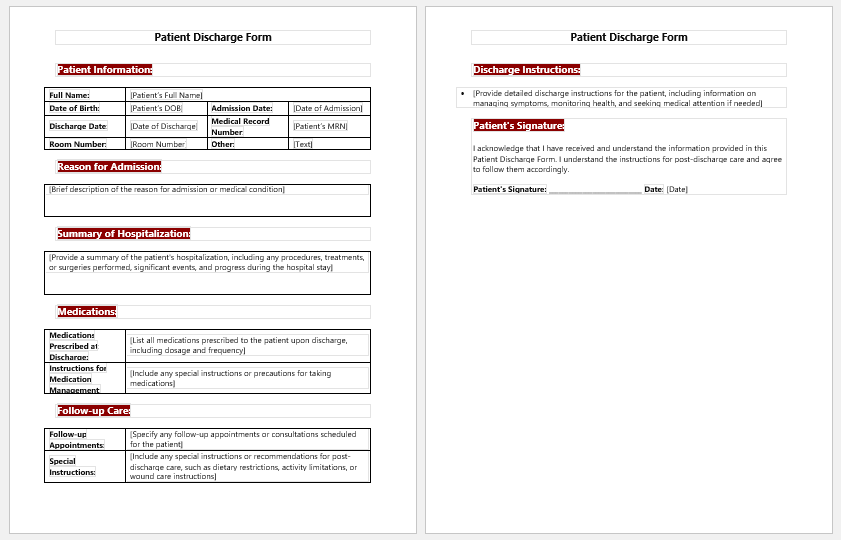
Components of a patient discharge form
A patient discharge form has to include all the basic information about the patient and detailed information about his condition, along with instructions for home. We will discuss them here one by one.
- Patient information: patient name, age, gender, and date of birth, along with their medical record number if issued by the hospital, must be filled in very carefully. This is a very serious matter, and we do not want to mix the patients with the same names. The patient’s contact number and email address, if any, are also very important to mention.
- Reason for Admission: Presenting the complaints of the patients for whom he was admitted to the hospital is a must, and all the details about his complaints are to be mentioned in the discharge form. That is why the history of the patient is always emphasized.
- Diagnosis at the time of admission: A necessary thing to fill out in the form is the diagnosis. Based on the presented complaints, a doctor diagnoses the patient, and this is the only justification for admission to the hospital.
- Treatment provided at the hospital: In the patient discharge form, the doctor has to write how he was treated based on his history, examination, and diagnosis. He has to mention all the drugs, whether oral, intravenous, or through any other route of administration, with details. If any investigations were done, they are mentioned in their final reports. If a patient is treated by surgery, the procedure and per-operative findings are to be written in the column of treatment at the hospital.
- Condition on Discharge: Being in the medical profession, we have to take every step carefully and document it even more carefully. The condition on discharge is a huge responsibility for the hospital and must be assessed and filled accordingly.
- Important Dates: Important dates like the date and time of admission, date of discharge, and duration of stay at the hospital are important to write.
- Medication on discharge: A patient, even if discharged from the hospital, is sometimes prescribed oral medicine to take at home. This occurs almost always in the case of surgical patients. So, it is the prime duty of the doctor to fill out this portion of the discharge summary with the proper name of the drug, the proper dosage, the frequency, and for how long he or she has to take this medicine.
- Instructions on Discharge: In the end, the patient is given some instructions on diet, activity, wound care, and following up on a plan for when he has to return for a checkup.
- Mental Health Evaluation Forms
- Forms Used by Pediatricians
- Various Forms Related to Pregnancy Verification
- Common Forms Used by ENT Specialists
- Pain Diary Worksheet Template
- Forms Commonly Used by Old Age Homes
- Medical Treatment Consent Form
- Home Exercise Program Worksheet
- Forms Used for Mental Health Assessment
- Forms Used by Psychologists
- Medical Forms Commonly Used by/for Students
- Assessment Consent Form
- Forms Used by an Anesthesiologist
- Not Fit to Fly Certificate Template
- Home Visit Consent Form for Schools
- Next story Consent of Treatment Form for Minor
- Previous story Dog Vaccination Form